You’re going to die after listening to this.
That’s a hard truth, but most of us don’t act that way. In this podcast, we talk to a couple of doctors that did.
And in doing so, found a way to align their passions with their paychecks. They found a way to love what they do.
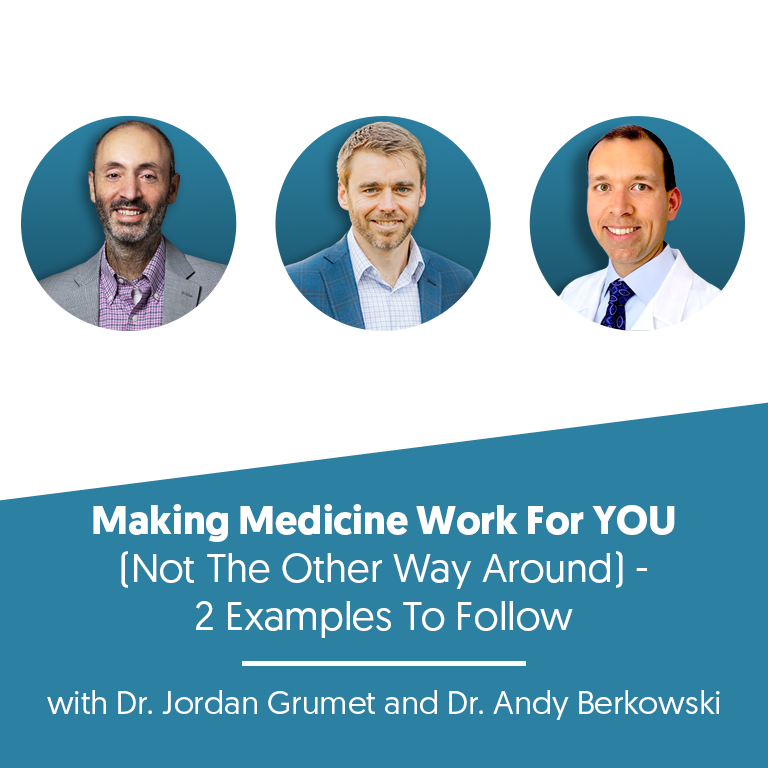
So listen in as we talk to Doctors Jordan Grumet and Andy Berkowski whose brushes with death gave them the courage to take real action towards finding true fulfillment in their work.
Dr. Jordan Grumet was a hospice doctor when he realized too many people waited until it was too late to live the life they truly wanted to live. This set him on a path to live his own life that way. He got his finances in order, reduced his workload for anything that didn’t fill his bucket, started leaning into things he was passionate about, and eventually became a full-time author, podcaster, and speaker with a side of medicine, not the other way around.
Dr. Andy Berkowski was a sleep doctor working in a research facility when he had a brush with death himself, facing a serious cancer diagnosis. He too got his finances in order and took different opportunities in research until he figured out that starting a direct care practice was the thing that would bring him the most joy and create the most impact.
You’ll see some recurring themes in these stories once they gain clarity-Getting their finances in order
Taking iterative steps toward their passions
Finally, understanding they could make their medical careers be the thing that supports their passion, not the other way around. We hope by listening to this, we help you gain the clarity that proximity to death gave them. But don’t forget, you have limited time to act…. Enjoy!
—————————————————————————————————————————
Transform your financial outlook today! Access our exclusive free resources for physicians and conquer financial stress. Access here.
- Connect with me on my LinkedIn
- Contact Finance for Physicians
- Finance for Physicians
- To schedule a call with one of our awesome planners, book HERE.
Full Episode Transcript:
You’re gonna die after listening to this. That’s a hard truth, but most of us don’t act that way. In this podcast, we talked to a couple of doctors that did, and in doing so, found a way to align their passions with their paychecks. They found a way to love what they do. So listen in as we talk to Drs.
Jordan Gromit and Dr. Andy Burkoski, whose brushes with death gave them the courage to take real action towards finding fulfillment in their work. Dr. Jordan Gromit. Was a hospice doctor when he realized too many people waited until it was too late to live the life They truly wanted to live this set him on a path to live his own life that way He got his finances in order reduced his workload for anything that didn’t fill his bucket started leaning into things he was passionate about and eventually became a full time author, podcaster and speaker with a side of medicine, not the other way around.
Doctor Andy Borkowski was a sleep doctor working in a research facility when he had a brush with death himself. Facing a serious cancer diagnosis. He, too, got his finances in order, took different opportunities in research until he figured out that starting a direct care practice was the thing that would bring him the most joy and create the most impact.
You’ll see some recurring themes in these stories once they gain that clarity. Getting their finances in order, taking iterative steps towards their passions. Finally, Understanding they could make their medical careers be the thing that supports their passion, not the other way around. We hope that by listening to this, we help you gain the clarity that our proximity to death gave them.
But don’t forget, you have limited time to act. Enjoy.
Our guest today is a physician, personal finance expert, speaker, author, podcaster, and entrepreneur. He’s been up to a lot of really cool things lately that I think are super relevant for this conversation today.
His podcast earn and invest, he talks about using money as a tool to pursue your purpose. He’s also worked extensively as a hospice physician and worked with many patients, you know, nearing the end of their life. And through that gained lots of perspective and it even inspired his new book, which is called taking stock, a hospice doctor’s advice on financial independence, building wealth and living a regret free life.
Our guest today is Dr. Jordan Grumman. Welcome, Jordan. Thank you for having me. I’m so excited for this conversation.
Also, as I was preparing for this song kept popping into my head and I had to throw this out there. It’s a Tim McGraw song, which is called live like you’re dying. I knew you were getting there. I heard it in my head. As you were saying, I was thinking of a song. I’m like, I’m hearing it. I’m hearing it. Yeah.
I mean, I kept thinking of that song as I’m like digging into kind of your message and what you’re all about. And it’s about a guy that’s like, gets the news. I’m sure all y’all listening have heard it. It’s about this guy that gets the news that he’s dying. And the way that he handles it is more of, you know, a positive view.
It almost looks at it as a blessing. And he goes skydiving, mountain climbing. rides a bull and loves his wife and all the things in his last few days or so. And it even, it ends out with like. I hope you get the opportunity to live more like you’re dying, which I, you know, it just kept kind of reminding me of this stuff, but is that how people actually, hopefully that’s how everybody is when they’re at the end, but is that how people are?
Well, I think it’s how people are in the end. The problem is it’s not how we are every day. So what I like to tell people is you are dying. It’s not if. You are dying from the moment you are born. So the question is, how can we use that knowledge to be more intentional about how we live our lives today? I think the Buddhists have the term memento mori, this idea of bringing this idea of your own depth into your daily life.
And the reason why is it’s really easy to put off those important things, right? Because important things tend to be hard. They’re difficult. They make us do uncomfortable things. Sometimes the things we really care about don’t go well with society’s norms. Maybe society says that we should go and be doctors and accountants and lawyers, but what we really want to do is be painters or artists.
So there are all sorts of reasons. To put aside those things that we really want out of life, as opposed to thinking about them today, the problem is, you know, we’re not guaranteed the days, weeks, or the years. My father died when he was 40 years old. Suddenly we never know when our last day will be. Does that mean we should sit there and worry about it every day?
No, but I think we should be more intentional about doing those things that are really important to us now. In your experience working with these patients on their deathbed. And I think, especially, I think of the people that were, I feel like it would be more real with the people that are aware of it, that kind of helped.
I guess you can relate to that more, but did it change you as a person going through that? And if so, like, what was that change? Oh, it changed me quite a bit. See, here’s the problem. When you have someone who’s dying and they get told you have weeks or months, all of a sudden they give them themselves permission.
To do or think about all those things that they truly wanted, right? They’ve been pushing all this stuff to the side because it’s scary or because it’s not what society or their family has asked out of them. So they’ve been not paying attention to their own real wants or needs. And now they’re told they’re dying and they say, okay, now I’m going to give myself permission.
Here’s the problem. You only have weeks or months to live. It’s really hard to kind of do those important things to get in touch with your sense of purpose, to get in touch with those people who are most important to you. It’s really hard to do that when you only have a short period of time left. What I call this in the book is the deuce ex machina.
This is the. Plot twist at the end of the movie that unexpectedly fixes everything. So in Hospice, we try to help people come to terms with their lives. We try to help them deal with their sense of purpose and what they mean in this world, but I’d rather avoid you needing the last minute plot twist. What if we started working on these things when we were much earlier and younger?
And so that’s what I kind of learned. How did this all affect me as I was dealing with the dying and I was seeing their regrets and I was seeing that they were scrambling to do these last important things in their life. Cause they never put the energy or time into doing it. I realized that I needed to look at my own life and instead of leaving it to the last minute, like they did, and instead of waiting for that last minute plot twist, I could start working on these things now.
I could start getting in touch with what was really important to me and then maybe living the next 30 or 40 years enjoying those things so that when I got to that point where a hospice doctor like me walks into the room to see me, I don’t have those kind of regrets that I so commonly saw in my patients.
What did that look like for you? Oh, for me, I think I realized that I was spending a lot of time doctoring and I wasn’t enjoying it. So by the time I got into hospice, the only thing I loved about being a doctor anymore was the hospice work. But I was spending 30 or 40 hours a week doing office work and hospital work and nursing homework.
So one big thing I did was slowly pulled away from those things. Luckily enough, I had built a financial framework that would allow me to do that. I realized that. I was more interested in communication and writing and podcasting and blogging all these things. I’d always promised myself when I had the time I would do, but the time was never there.
So I always wanted to write a book. I always wanted to do things where I could have these important conversations that would help people. But I kept on putting it off because I was too busy being a doctor, making a living. You know, being my profession. And so I think dealing with my dying patients with these hospice patients helped me finally cleave that bond to these things I thought I was supposed to be doing and start really questioning, well, what do I want to do?
It’s so interesting that we’re chasing this whole, like a lot of us are chasing retirement or happiness or whatever. And we’re working so hard, but we don’t even have any space so much that we don’t even have any space to enjoy it today. And so it’s all kind of like future focus. Which is interesting because what’s the point of retirement?
I mean, a lot of us think of retirement or think of getting to this place where we call financial independence or financial freedom. And we almost focus on that thing, the word retirement or this idea of financial freedom. But we don’t think real deeply about what that gets us. What it should get us, retirement or financial freedom, is the time and the space to do those things that are purposeful and meaningful to us.
But why do we have to wait to retirement to do that? Why can’t we start thinking about those things when we’re in our thirties and forties? And so your average person would say, well, we’re too busy working or building a family to do that. But I would argue, well, why can’t we incorporate those things into our work, into building a family?
Why do we again, have to focus on the purpose of work is to make money. And the purpose of having money is a goal so that I can stop working. That all sounds great, but. Again, it’s this idea. Money is a tool. We work to build up more of this tool, but then we have to make sure that we use that tool to actually do those things we want to do in our lives.
Yeah, I think, I think most people will say, Oh yeah, I get it. Like money is a tool. But then if you look at their. They’re kind of caught in this pursuit of more money or the money is the end goal. So there’s this disconnect. It’s really easy to make money of the goal. And think about this. Money is easy because it’s quantifiable.
You can measure and monitor it. You can set these wonderful goals and then something happens. You reach your money goals. If you’re lucky, right? You get to that money goal. One of two things happens because you made the money, the goal. Once you get there, you feel empty because you’ve met your goal and you don’t really have anything.
It’s not meaningful. It’s just a number on the bank account. So what some people do then is they just double the goal, right? So I wanted a net worth of 500, 000. I got there. I don’t feel happy or wonderful yet. Something still feels off. So what am I going to do? I’m going to make my goal a million dollars.
That’s one problem. The other problem is let’s say 500, 000 is your goal and you get to 500, 000 net worth. All of a sudden you get petrified, you’re going to lose it. And it’s something called loss aversion. This idea that we’re doubly afraid of losing what we’ve gained. Then we are of never gaining it in the first place.
The reason why reaching these money goals causes this anxiety is because they’re hollow. They’re mirages. It’s just a number on the paper. It’s just this thing. That we’ve created to mean value or wealth. These are hollow goals and they don’t make us feel good. What we need to start doing is thinking about, well, what’s really important in our lives.
What do we want to accomplish? And once we move past that, then we can see what money can be used to do for us. And these are more durable, tangible goals that actually. Give us some modicum of happiness versus just some net worth number, which we think is going to make us happy, but actually most people get more anxious as they get closer and closer to that money goal.
Yeah. And I think the science backs up a lot of research has been done on that. And I think it all backs this up. I’m curious if some of these people nearing the end of their life, were some of them, you know, doing it right. Like had some of them kind of like, really just, you know, knocked it out of the park on like.
They were in touch with their purpose. There are plenty of people who live really good deaths. I’ve highlighted in the book, a lot of people who had regrets. And the reason why is I wanted to show how these regrets could translate into making a better life for us as people when we’re younger, but the people who start thinking about purpose, identity and connections early on in their life.
Actually tend to get to the end of life and don’t have these regrets. There’s not the mad scramble to accomplish all these things because they already have, but it is still the rarity in the sense that most people don’t really want to face these tough questions of what’s really important to me and how do I achieve it.
Most people put it off. And I think a big reason people put it off is because it’s scary. Like when you start thinking about meaning and purpose in these big things, it reminds you that life is finite, that you could get to the end one day and not meet these goals. And that’s really anxiety provoking to think I could die one day.
Maybe I won’t achieve what I want. So instead of even thinking about it, people just put it off and concentrate on the easy stuff. I think money is an easy thing. It might not be easy to make money, but you know, the steps like, you know, I could get a raise at work. I could get an extra job. I could start a side hustle.
I could invest more aggressively. Like these all are. Answers to simple questions. But then when I say, well, who do you want to be in? What do you want out of life? That’s a much difficult question. I think it provokes a lot of anxiety. And I think some of that anxiety is tied to the fact that it reminds us of our own mortality.
I mean, it’s an evolving thing. If you’re kind of caught up in this. perfectionist mentality. I think it’s like there’s no perfect answer for that. It’s like impossible to perfect your purpose and future self and it’s evolving over time. Do you think there’s specific challenges physicians face? Ideally, we’re all living a regret free life, but as a physician, do you think it’s particularly challenging?
Oh, I think it’s very challenging. One is there is a huge societal pressure to be doctors and what being a doctor means. So anyone who wants to step out of that narrative really faces a huge backlash. The other problem is what most of us go into. Medicine for this dream of being there and helping people and making a difference that dream gets a little bit mangled as you go through medical school and residency.
And by the time you come out, you realize what you’re doing for a living isn’t what you thought it would be. You’re spending a lot of time in front of a computer. You’re trying to help people who sometimes don’t want to be helped. You’re arguing with insurance agencies all the time. And so burnout. While common in all fields, I think is extremely important in the practice of medicine because it’s so, so common and so, so easy to become a victim of it.
So I think that’s very unique that we decide usually at young ages that we want to become physicians and. There are all these societal and external pressures that push us onto this path. And once you’re on that path, it’s really hard to veer off. Not to mention that if you do end up being a physician, you finish residency, and you’re like, I hate medicine.
I don’t want to practice it anymore. Guess what? You might have hundreds of thousands of dollars in medical school debt. And the only thing you know how to do that creates income is be a doctor, which by the way, creates lots of income. So if you’re going to step away from that. And then go do something you’re not nearly as trained to do.
You’re not going to make as much money. You’re going to have a hard time paying off those debts. Yeah. It’s a challenging spot to be in. How do we start to gain greater awareness or start to maybe, I mean, the burnout situation is challenging because I think if you’re in the rat race and you’re just grinding it out, it’s hard to even think straight.
And so maybe it depends on circumstances, but like, how do we start to kind of move the right direction on this? So I think the first step is you almost have to take your finances and put them aside for a moment, which scares everyone, right? Because I’m someone who’s interested in personal finance and I’m actually telling you ignore your finances for a short period of time or put them on autopilot for a short period of time.
And the reason you want to do that is you really need to start thinking about what do purpose, identity and connections look like in my life? What does meaning look like in my life? Only after you do that really hard work, which sometimes takes months or years, can you then go back to your finances and say, okay, I know who I want to be.
I know what I want my life to look like. I know how I want my days to be filled with meaning. Then you need to go to your finances and build a financial framework that fits around that. Now, of course, that leads to a very difficult question, which people struggle with all the time is, well, how do I define?
Find my sense of purpose and identity. And that’s a whole nother conversation that gets into what we were talking about before with things like a life review. There’s lots of exercises we can do that help us start getting in touch with who we are and what we want out of life that help us see through that kind of mirage of wealth.
Let us see past money and net worth and start thinking about the more important things like how do I want to spend my time? What do I want to contribute to the world? Who are those people I want to touch in? In what way? How do I want to be remembered by my children and grandchildren? All of these kind of big questions get us past money and make us think about what’s really important to us.
Yeah, I think the natural tendency is to Focus on the money first, like you’re saying, I was looking at some of my goal setting from when I was early in my career. And it was exactly what you’re talking about. It was like a, you know, net worth and income. And then I think I had like a five year goal of like needs to work on.
Relationships and spirituality or something like that. And I’m like, well, I had it all backwards and I think that’s common. I think it’s really common. And again, it’s very comfortable because if you think about your list, you knew the steps to take to get to a higher income or to be higher on the professional stratosphere, whatever was important to you there, but it’s kind of amorphous when you start saying, well, how do I become more spiritual?
How do I work on my relationships? Like that stuff is. More difficult, more time consuming, and in some ways more stressful. So it’s easy to put it aside. But again, when you flip the script and you realize that money is just a tool to get you to those other things, then you realize, well, I need to know what those other things are first, before I then build this tool to support it.
How can we know if we’re headed on the wrong path? Either I think of maybe symptoms that we can say, you know. Maybe I ought to really, because it’s hard to self diagnose this kind of thing, and but I’m sure there’s kind of like warning signals. You know, it doesn’t feel good. So let me tell you about what happened to me.
I had been identifying myself as a doctor for most of my life. My father died when he was 40. He was an oncologist. He had a brain aneurysm. He died while he was rounding at the hospital. I was seven at the time. And like lots of little kids, I somehow convinced myself it was my fault, right? As a kid, you see everything through your own lens.
And because it was my fault, the way I was going to make up for this was I was going to become a doctor and I was gonna fulfill the role that he couldn’t because he died young. And that became really purposeful. And even in some ways, joyful to me, this is what I was going to do for a living. I would do it.
Even if you didn’t pay me, this was the thing for me, it was very purposeful, but something happened. You know, I went to residency in medical school and I had almost no medical friends. All my friends were excited when they became residents because they could hang out in the doctor’s lounge and I felt so uncomfortable there.
And finally, when I was a doctor and I was practicing my wife and I would go to parties and we meet new people and I would almost be embarrassed or ashamed to tell people what I did for a living, which is crazy because there’s nothing. Shameful about being a doctor. It’s a very proud profession, but what I realized is I was wearing this identity on the outside, like a cloak that didn’t match my identity on the inside.
And so I had to do a lot of work to figure out what my identity on the inside was. And I realized that it was as a communicator, a writer, a podcaster, a public speaker. Once I recognized this disconnect. I realized how uncomfortable it was making me feel. So how do you know you’re on the wrong path? It doesn’t feel good.
You feel disconnected. You surround yourself with peers who are excited about the things you like to do, but you don’t see or feel the same joy they do while doing it. Because you don’t fit. And so you have to start looking for those signs that the path you’re taking doesn’t feel comfortable or good, or isn’t really meeting your needs.
And then the hard part starts, right? You got to make changes potentially. So what did the work look like for you when you started to, you saw the signals, which is huge because a lot of times we miss the signals. I think we get the signals. Most people they’re all over the place, really, but you saw the signals.
And then what did the work look like? So, I had an epiphany. I realized I was burning out of medicine. It was stressing me out. I knew, I just knew I couldn’t do this forever. So, I started looking at my finances saying, well, how do I get out? How do I have enough money to support myself so I don’t need to work again?
I was struggling through this and this guy, Jim Dolly sent me his book, the white coat investor, which is a book for high net worth individuals, especially physicians. And I read his book and it gave me the vocabulary to understand my finances. And I realized that I actually had enough money. Like he gave me the words and the equations and everything.
I said, wow, I have enough money. I could stop working as a physician right now. And I would be fine. Which felt great for a moment. And then I had a panic attack because the only identity I had ever had, the only connection to my father who died when I was a little boy was all tied up in this profession.
So I was lost. So this is what I did first and foremost, since I had some financial power. I looked at my job of being a physician. I started getting rid of things that didn’t fit that were causing me stress or causing friction in my life. So I call this subtraction. I started subtracting out the biggest pains in my job.
So at that time I had a private practice. I wasn’t willing to step away from being a physician. Totally. I couldn’t step away from that identity. It was just too fresh and new and I didn’t know who I was. But I could get rid of my practice, which was calling me all sorts of stress. And I was going to patients houses on Saturdays and Sundays to see them.
So I got rid of that and I was doing nursing homework and hospice work. Over a year or two, the nursing homework got more stressful. I was getting calls at three in the morning. So eventually I got rid of the nursing homework. I was lucky I had enough money. I could do these things. Eventually I kept hospice work and the thing about it was hospice work was work.
I would do even if I wasn’t being paid for it. So that was a big sign to me. I said, okay, I started getting rid of things I didn’t like in my current workplace and what I was left with is something that felt genuine, purposeful, something I would do even if I wasn’t being paid for it. So I kept that, but I even hewed that down further.
I got rid of nights and weekends and being on call. What I was left with is 15 or 20 hours a week of mostly being in meetings and taking texts. But otherwise I could build it into exactly what I wanted it to be. So for me, I subtracted out all those things I didn’t like about my job, all those things that were causing friction.
When I did that, I went from working 60 hours a week to working 15 hours a week. All of a sudden, I had all this free time. So the question was, what were the things that were meaningful for me that I now had time to do, which I never had before. Of course, there was the obvious family stuff like being there for the kids and my wife and et cetera.
But what I really recognize is all throughout my career, I was squirreling away little bits minutes and hours to write blogs or do public speaking or to act as a communicator. I was squirreling away these little bits of time to do it while my family was sleeping or during an odd lunch break here or there.
And I love doing these things and I would call it a hobby because I told myself, well, you can’t make a living doing that. That’s not what you do full time. That’s what being a doctor is. When I realized I now had all this free time, that was what I wanted to spend more time doing. So it was epiphany to me in the sense that I could actually start doing those things that I would always consider hobbies, the things that really I was passionate about, and I could spend more and more time doing them.
And once I started doing that, they became really, really purposeful for me. And so that’s how I had to approach it. I had to do it slowly. I had to get rid of those things. I didn’t like first, create some time and space, and then start slowly adding in those things that are purposeful to me. Now, a lot of people could be listening to this and saying, well, most of us aren’t as lucky as you are.
Maybe we don’t have hobbies. Maybe we don’t think. Or know what’s purposeful to us. But for those people, I’d say, well, now you have some extra time and space in your life, start throwing the spaghetti against the wall, start volunteering for things, start thinking back to childhood and what really got you excited or motivated.
Think about those nights where you woke up in the middle of the night, excited by an idea and your heart was racing and you couldn’t fall back asleep because it was so cool. Well, did you pursue those things? Maybe you convinced yourself the next day you were too busy or it didn’t fit into your work schedule, or that’s not what adults do.
But now if you can create some space in your life. Maybe you can start pursuing those things and start thinking about what do I really want? What really gets me excited?
Let’s take a quick break to hear from our sponsor, Wren Financial Planning. Want to hear something cool? My team at Wren Financial Planning has consistently told me that the listeners of this podcast are their favorite people to talk to. Did you know that you can set up a no cost triage meeting with one of our amazing CFPs at Marin Financial Planning anytime and talk about your biggest financial questions?
We can discuss things like considerations for transitioning into practice, getting the best bang for your buck buying a house, the smartest way to pay off student debt, or tips on maximizing your compensation package. Or maybe you’d love a second set of eyes to help look over your tax return or investment allocations.
Maybe you’d just like a general second opinion from your existing advisor. Either way, our role in this meeting will be to listen to your concerns and help you start to identify potential actionable next steps. So that you can start to make solid progress, addressing those concerns as quickly as possible.
Schedule a meeting. Now you’ll see a link in the show notes. And when you do make sure to indicate you found us from finance for physicians. We look forward to talking to you. Okay. Let’s get back to our show.
Andy, thanks for joining me today. Welcome to the podcast. Oh, it’s my pleasure. Thanks for inviting me. Yeah,
I think it would be good if you could kind of give us a little bit of a backstory on you, like kind of how you got to where you are today. Yeah. A lot of this is very Much on the things you’ve talked about in previous podcasts, particularly about the rate of burnout, the unhappiness among physicians, the fire movement.
So, I guess I could take you back to about four or five years ago.
So, I was working as a sleep physician at a very large academic center, and I was a few years into my practice, and oftentimes changes are made through sentinel events. And I had a series of sentinel events. The biggest one is Out of the blue, I developed a life threatening form of cancer, and this was back in 2018.
And so, for your audience, you know, a lot of the things you’ve touched on, the time to get disability and life insurance was yesterday, because I basically had no health problems, maybe a little overweight, maybe very, very stressed out at work, so those were my risk factors. But I’m facing a life threatening cancer and I’m not prepared financially for it.
And that kind of made me reflect both on how I was living my life in terms of what I was doing as a career, how I was spending time with my family, and that was probably my sentinel moment. I wouldn’t be here where I am today had that not happened. And given that I am still here today, five years later, I survived, obviously.
But it was a poor prognosis, a rare form of cancer, and I had a 50 percent chance to be here in five years. And, you know, through God’s plan, I’m still here, and I’m better off for it. What happened during the year, I was basically off work for maybe almost nine months, and I didn’t actually have disability insurance, or at least private disability insurance.
I’m married to a another physician. So my wife works very, very part time as a pediatrician. And our plan was, Hey, we’re going to just anything really, you know, unlikely were to happen. You could always just work full time. You know, that that’s easy. She’s the insurance. Something happens to me. And well, while I was reflecting on this during my year, where I was basically in the hospital for more than a month and a half and getting chemotherapy and surgery.
I thought to myself, well, that, that’s bad because my wife’s not working now and she can’t take care of the kids because she’s taking care of me and she can’t work because she’s taking care of me. You know, it would be nice to have a disability plan and we did have one through the university, but that was limited.
That could have run out. In fact, it almost did run out and I had nothing in place and that, if that’s not a side lesson to your audience, I don’t know what would be because. I was a healthy person and all of a sudden I could be dead in less than a year. So, that’s probably a common story for people who develop cancer, but I, I did not see that coming, obviously.
But fortunately, I, I survived the whole process and I went back to work in my academic practice and it really gave me a new perspective on things, particularly a focus on my personal health. and my family life because the biggest factor was I think the high levels of stress in my job were one of those risk factors for cancer.
You elevated cortisol levels. A lot of your physician audience will know all of these things that happened to the body when we’re under high levels of stress. And being a sleep physician, I’d always thought I’m going into the lowest, lowest acuity field in medicine. Like all these disorders are chronic, they’re lifelong, nobody’s really dying of these things, there’s no emergencies.
And yet I was completely stressed out in my work, and that gets me to the system. I thought at that point, Hey, I’m cutting back, I’m going to cut to 75%. And you know what? 75 percent of miserable is still miserable. Okay, so it didn’t matter that I cut back from 100 percent to 75%.
I was still, you know, almost working, you know, close to 50 hours a week, still working on weekends, even though I apparently got an extra day and a part of another day off. It really wasn’t the time. Much less like what you’re actually doing with that time. And that’s really where things started to change for me.
Because I was given a second life. And I wanted to make things better the second time around. This was my second opportunity in life. And it turned out that I was focusing on a condition. A lot of these conditions, particularly the one I, I’m a specialist in, which is Restless Legs Syndrome. And Restless Legs Syndrome, Is not valued in the insurance based medical system.
So at the academic center, even though I was an expert in this area, doing a lot of good work in this area, I wasn’t really valued as a physician. I was pretty much overworked, not much time for research, not much time. For teaching and I was kind of low on the totem pole. So I was not getting the good assignments in terms of teaching assignments and clinic assignments.
So I was working really hard and I wasn’t doing the type of work I wanted to be doing. I was doing research on Saturday morning and, you know, here in Michigan, it’s, you know, snowing today. I was spending my 70 degree Saturday mornings in May, instead of playing with my kids outside, I was, you know, writing research papers, and that’s not what I thought I would be doing when I went into academics, because part of the sacrifice of academic medicine is your salary.
So the salary was close to the first or second percentile for this specialty. So. And yet I was working as much as many other physicians who would make maybe two or three times as much. So I’m taking a financial sacrifice. I’m miserable. I’m not actually doing what I think I’m doing. I think I need a change of scenery.
So that’s like a direct conflict of your values. Complete direct cause I thought I would be doing a lot of teaching and research. And you know, the sacrifice for that is you go to an academic center, you take a lower salary to do that. But now I’m taking a lower salary, but I’m basically working private practice cause I’m not doing any teaching and I’m not doing any research.
Except on my own spare time. So it really wasn’t what I thought I would be getting into and it turns out that that wasn’t unique to me as I’m sure some of your guests have already talked about and, and the way the system is even the academic centers now are becoming businesses, they’re becoming businesses where they’re making Their product being medical services and their full goal is to make money.
It’s not to teach, it’s not to do research anymore. And these are the most academic of centers. If they’re not doing it, certainly not the private hospitals and large physician practices are focused on. Teaching and research. So it was kind of a crossroad situation. So I was at a conference and I was sitting next to a primary care physician at the conference And I don’t know why we were talking about it, but we’re talking about preventative medicine and she told me hey, this was dr Taki, I could you know reference her but she said oh, I I just started a preventative care practice It’s it’s sort of lifestyle management practice.
I said the first thing I thought of is how can you do that? What? The insurance isn’t gonna pay for that. How could you even spend an hour talking to somebody about preventative health care? And she said, no, I’ve started a clinic. It’s called direct primary care. And I, this was a few years ago. I had no idea what this is.
So getting to talk to her, she actually inspired me to consider going into this area. And So what happened was she had connected me with a consultant who sets up a lot of these concierge direct care practices. I was in talking to him about ideas. He thought this would be a great idea for me. And he was right.
It was a great idea. But what happened was I’m sitting here with no life insurance, no discipline. I had life and disability insurance, but it was through the organization. I didn’t have independent life and disability insurance. So now I’m coming a few months off of a life threatening form of cancer. I might not be alive in a year.
Am I going to go off and start my own primary care practice with no protection for my family? The financial, I guess, it wasn’t a mistake. It was like a financial lack of awareness back then. Cause me to change how, you know, what type of career move I made. So I said, that’s a great idea. I can’t do that. I need to take a job at a major medical center where I’m going to get life disability insurance.
I’m going to have a salary, you know, annual salary. I can’t afford to take this risk. And so that’s what I did. I ended up right before the pandemic, taking a second academic job. And it turned out it was the exact same experience, if not, no more extreme than the first one. So it wasn’t just. the medical center, bad luck.
I go to a second academic center. It’s the exact same experience. And I wasn’t being valued for treating a condition that is not reimbursed. So like not having your finances exactly in order kind of put you in a position to have to continue to conflict with your values, essentially. Well, exactly. So if, if I had something as simple as life and disability that I could just carry with me into my own practice, if I dropped dead of cancer in three months, my wife and family are fine, you know, and so that actually made the decision.
So I went into a second job, mostly because I didn’t have my financial ducks in line. How did that feel in the moment? Like, well, did you kind of, were you thinking a lot about that? I’m assuming a little bit. I was, that, that was the kind of the clincher in the decision, but I also thought, Hey, I’m going to this new center.
They promised me we’re going to focus on this area of research for you. Because I had only been I had worked also at at the V. A. So I had been in a V. A. system and academic system, but I hadn’t been to a 2nd academics. So I thought, well, the 2nd academic system got to be better than the 1st 1 right? And it really was not.
It was doubling down on every, you know, just a microcosm of what’s wrong with medicine. And the fee for service insurance based system that’s going on at that point, really, actually, right before I took that job, I had a friend from he was a friend from residency and then also was had joined the department where I was working previously.
And he’s like, Oh, you need to, you know, become more financially literate here. Listen to this podcast. And one of them was called, you know, the white coat investor you’ve had Dr. Jim Dalian in the past. And so I, I’m like, why, why would he, I’m getting a new job. Why do I need to listen to this finance podcast?
And I didn’t make the connection until. Maybe a couple months into it about how important this financial literacy would be to how you can You know the flexibility in your job and in your career and that one and and ryan inman’s old financial residency podcast Those I was starting to like gobble that stuff up in this transition and that actually has what?
set me up for the next career change, which is what I’m doing now, which is starting my own direct specialty care practice. Because less than two, maybe a year into my second academic position, I knew that that wasn’t for me at all. And I thought about going to a third academic center, but then I thought they’re all going to be the same.
it’s really not a system that I’m thriving in. And maybe a background for your audience is, in my opinion, in each specialty, the entire system of insurance based medicine is designed on the number of procedures you do, whether it’s diagnostic or treatment procedures. So it’s biased to doing things for people that are measurable in this procedure.
And we have procedures in sleep medicine. They’re called sleep studies. But what are the conditions that don’t involve sleep studies? Well, restless leg syndrome, it’s a neurologic condition. where there’s no diagnostic test and there’s no treatment that’s in a procedure. Insomnia. Insomnia is behavioral lifestyle changes, no procedure.
Even a sleep study is pretty useless when it comes to insomnia. So you wouldn’t guess these are two of the three most common sleep disorders, but they’re completely neglected in our field. The number one treatment for insomnia is a therapy called cognitive and behavioral therapy. There’s maybe 10 people in the state of Michigan that do this, and like 10 percent of the population has insomnia.
So how can you have this first line treatment, but nobody actually does the treatment? Well, because nobody’s reimbursed for the treatment. It’s all done by social workers and therapists. Not one physician that I’m aware of in the state of Michigan does cognitive and behavioral therapy for insomnia. So you got this disconnect of the system with the actual science, the actual treatment of the condition.
And that was true for my biggest specialty, which was restless leg syndrome. And because it wasn’t valued, I felt like, hey, how can I serve my patients, particularly the complex ones who are being ignored in the system? I can create a practice. where they actually would pay to get the treatment that they deserve.
And that’s how I, I could reason it from a business standpoint. It’s that the system, you, you could get certain care through the system. These other neglected conditions, maybe people would actually pay outside the system to just get the treatment that’s not available in the system. And that’s what I was banking on.
There were a couple of funny days that really convinced me of this. There was one day I became this kind of regional expert in restless leg syndrome. So this one clinic day, I had two patients on the same day. One, she showed up in her, in the room and she had a suitcase. I said, why do you have a suitcase here?
She’s like, oh, I’m just coming from the hotel. I’m going to fly back after the visit today and she was from Florida and I said, huh? Well, so I’m in Ohio at this point, okay So I’m in a clinic room in Ohio and and she’s flying in from Florida to see me There are no other physicians in Florida that can treat this condition.
So you’re flying to see me Maybe instead of flying to see me She would pay money to see me through telemedicine and not spend the time on the flight and the hotel fee Maybe next patient after that patient drove from Milwaukee all the way to Ohio, skipped all the academic centers in Chicago, Indiana, all the way to Ohio to see me in person outside of her state.
So, so this kind of reinforced that there’s this demand out there for good treatment. And maybe patients are willing to bend over a little bit, maybe bend over backwards to get it outside the system. So that was really the impetus. That’s where I thought from a business standpoint, direct specialty care can work because we had only heard about it really through direct primary care, which makes sense.
You don’t want a 10 minute visit with your doctor. You might pay a monthly fee. To actually get good care for like an hour Whenever you need it and have a personal relationship with your doctor like how it used to be But for specialists specialists, we do all the procedures. Why would we need to leave the insurance system?
But within each specialty there are these hidden conditions that are not profitable In the current system and they’re ignored and neglected and there’s a huge market for that and this was my business justification in in part and so So that’s kind of where I got to the point where, Hey, I could either take another academic job and it can be the same miserable experience, or I can start my own practice.
And I was actually inspired by my mother. So my mother started her own business toward her retirement years and, you know, not to coincide with finance stuff, but she, she’s an investment manager. So I know half of your index fund audience is cringing. She’s a portfolio manager. So she invests in stocks, small groups of stocks for.
People who are investing money. She started her own business long after she, after the kids were out of the house and, and my dad was close to retirement. I said, why should I wait my entire career to start my own business? I can do it right now. My mom can do it. Why can’t I do it? And my mom’s still, you know, she’s at Fern Capital Management.
She runs her own business still, like right now. So why can’t I start my own business? I’ve got my whole career ahead of me, hopefully. So she inspired me to do this. So it was a constellation of things. It’s these direct primary care doctors who I’ve been talking to. financial literacy, the FIRE movement, being wise with your finances, but not a FIRE movement to retire immediately, but a FIRE movement to have flexibility in what you do.
Because if you have financial flexibility, you can take a risk and start your own practice. Because with, with my current direct specialty care practice, If I went out of business, guess what? There’s a shortage of doctors. I could just get a regular job, you know, within a few months, I’m not going to be in big trouble.
But if I, if I don’t have my financial ducks in line. I can’t do that. So so that’s kind of the sort of the confluence of the system being broken Becoming financially reasonable as an individual and being entrepreneurial and I think that’s possible for many many doctors who are upset with the system.
Yeah. And it’s, uh, it’s, you’ve kind of described it well. I think it’s multifaceted in like, it requires varying skill sets and they apply well to life too, like financial literacy, I would advocate for anyone. Whether you’re starting a business or not. I mean, that’s like just a very foundational healthy thing to do.
And even, you know, having a focus on health and family, like I think it’s difficult for a lot of people to that are like stuck in the grind. And in conflict with their values to even get enough of a second away from that grind to even like think about like what’s most important and I’m actually aligning with it and how do I do something different to kind of get away from that?
So it’s a lot of different factors that kind of have to come together and then you have to get. Prompted with these ideas, like you said, you happen to be introduced to the idea and sitting next to a colleague. That’s, I mean, that’s fantastic to kind of get that. It’s like the seed gets planted right there.
And then all these other things start happening that like germinated, you know. It’s growing all of a sudden, and then boom, you’re rocking a business. I think when you’re looking at it on the front end, it’s super scary. A lot of people, I think fear is the number one thing people deal with when they start.
I bet people listening right now are like, Ooh, that seems scary. But I would kind of take a step back. Like the, the problems, I think a lot of people I see. Going through in healthcare are also scary and in conflict with your values, you know, like having that be, I mean, what’s the cost of working in a environment that forces you to conflict with your values and over a lifetime?
I mean, over a career, I mean, what’s the, that’s a huge and when you kind of start to look at it a different way like that, that can kind of. Get you that motivation. It seems like for you, it was just a combination of factors that gave you that courage, like, or was there this, I mean, was it your mom? Was it just, or was it a combination of everything that kind of came together to give you that motivation to kind of go into the unknown and take the risk?
Well, yeah, it was a combination. Cause you, you can’t do things where you don’t have. People have gone before you. I guess in some ways, this is there in terms of direct specialty care. I’m only aware of about three or four sleep direct specialty care clinics, and they’re actually growing now, but but there’s not a lot of people in my specialty, but there were other specialists out there.
The direct specialty care alliance had a listing of doctors, and there were maybe five, six or seven at the time, and that’s grown even since I started my practice. So, um, yeah, But I went to their websites, I said, Oh, wow, there’s a cardiology physician doing this. There’s a podiatrist. These are procedural based fields and they still are finding a way to do, well, because cardiology is a lot of procedures, but what about preventative cardiology?
What about neurology that involves long term management of things like migraines or other neurologic conditions that don’t involve procedures? Rheumatologists who, who involve, manage these chronic conditions that have no procedures involved. So I said, well, they’re able to do that. It actually was inspiring to see just a handful of people in the country doing this.
And then you, you obviously have the direct primary care groups that are, I think, growing exponentially. There’s no doubt that direct primary care is going to work in most cases, but for direct specialty care, that’s relatively even newer concept. And With the patients I was seeing, I was restricted to these, like, 20 minute return visits, so I got, I even had a patient from your, you know, Lexington drive up to Cleveland, 6 hour drive in a 20 minute slot.
You think the patient deserves a 20 minute visit if she’s going to drive 6 hours to see me? And I needed 2 hours with her. So I said, why can’t I create a clinic where the patients get the time they need, they get the follow up, and they get the correct management of their conditions? Because a lot of this is, like, the conditions are being mismanaged because people just don’t have time, time to see the patient.
Time to go over behavioral modifications of things that are time consuming and don’t have time to read about the conditions because they’re on to the next patient, they see 30 patients a day. You don’t have time to read about something new you ran into at the 8 o’clock patient if you have an 8 15 patient right away.
So, that system was so oppressive to me. I couldn’t just do a 20 minute visit. I, I have to have time with the patient to get it right. And I, I talked to some of my colleagues from fellowship and I said, Is there something I’m doing wrong? Can I be? Super efficient and see these patients at 20 minutes and they’re like, no, you can’t provide good care without time, no matter how efficient you are.
And, and the system that involves volume of patients is in conflict with high quality care, which you can’t get around time, education, counseling, behavioral modification. That stuff is fundamental to health and you can’t be super efficient and get that done in 5, 10 minute visits face to face with patients.
So I either had to compromise my care or find a system or leave the system. So what I did was I was thinking about leaving the system. I had looked at non clinical jobs like many. People in your audience have done and that that be side gigs, but even side gigs as a as a full gig that’s become really popular, unfortunately for doctors and so that the direct specialty care route ended up being the kind of escape valve and I’m almost a year in now and I cannot believe how liberated I feel.
Like, I’m, I am so excited. I almost wanna work more than I do when I used to, you know? Yeah. It’s crazy. I actually wanna, I can’t find enough time to work now and because I want to do it, I’m so excited about the type of work I’m doing. It’s, it’s been great. So I, I don’t know if you want to kind of transition into the type of practice I’ve set up, or, you know, yeah.
I mean that, that, I can so relate to that for me. So I kind of had a similar experience in my career and what I had like a more of a ultimate like. Like when I came to grips with this idea in my head, it was over, game over. And the idea was that I realized in financial services, the traditional system, that I couldn’t provide the best possible advice for my clients.
And there was an alternative where I could do better. And when I kind of came to that realization, I’m like, I’m out. I got to go today, you know? So it was very quick after that. Realization. Cause I think most physicians I know are very dedicated to like the patient and taking good care of them. And I think if you can come to that realization that.
And I mean, in some cases you are able to provide the best care. I’m not trying to say physicians aren’t able to provide the best care, but in a lot of situations you’re not. And if you can admit that to yourself, the system is not going to want you to admit that, I don’t think, because there’s a there’s an incentive to continue to have you there.
So you it’s kind of have to. You have to do that hard work yourself. It’s a complicated thing. I mean, you have to look at yourself. You have to look at your finances. You have to look at, you know, what’s most important. And that’s why your story is so great is you kind of had all these experiences and looked at all these different areas of life and you had this wake up call too, that was kind of like a.
You know, second chance at life, which, you know, really, I’m sure, really emphasize that importance of, you know, time is, you know, life is short and you never know what could happen. So what’s the point of working in a terrible job that conflicts with your value, especially if you don’t have much longer to live?
I mean, family, I know you’ve already said family’s important and, you know, you got to carve out the time, but now it sounds like you’re on the other side of the coin. And that’s what. I’ve heard this story over and over again. It’s like, when you can get in a place where you professionally like start to love your work, then it’s totally different.
You still have these pools between like life and family and, you know, all these different values, but like the work thing is pulling at you because you love it and it’s. Reenergizing.